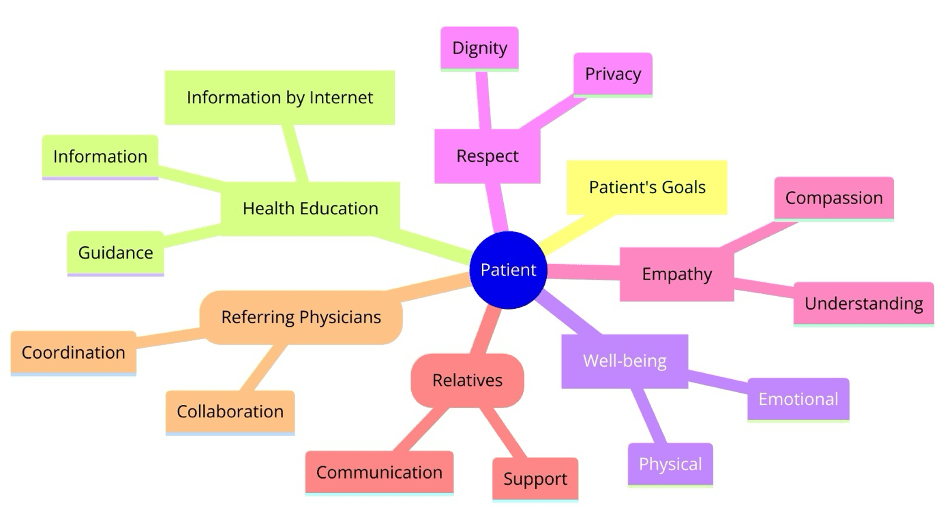
Communication in healthcare, particularly in fields like interventional radiology (IR), plays a pivotal role in patient care, treatment efficacy, and the overall healthcare experience. This session will delve into the nuances of effective communication between interventional radiologists, patients, their families, and referring colleagues. We will explore verbal and non-verbal communication strategies as well as the impact of internet-based health information, and provide targeted tips for working with cancer patients and their families as well as with referring colleagues.
How does a patient feel when communicating with an IR?
For patients, communicating with an interventional radiologist can be a daunting experience. The complexity of diagnoses and the uncertainty of procedures can evoke feelings of anxiety and confusion. Effective communication by IRs can significantly alleviate these concerns, making patients feel heard, understood, and valued. It is therefore crucial for IRs to bridge the gap between medical jargon and the patient’s understanding, ensuring they feel comfortable and informed about their treatment options and what to expect.
Verbal communication: from medical to everyday vocabulary
The transition from medical to everyday vocabulary is a skill that IRs must master. Simplifying complex medical terms without diluting their meaning allows patients to better grasp their health situations. This does not mean underestimating the patient’s ability to understand, but rather adapting the information to be more accessible. Effective verbal communication also involves active listening, patience, and the ability to provide clear and concise explanations.
Beyond the words: the basics of non-verbal communication
Non-verbal communication, such as body language, eye contact, and facial expressions, and even the physical environment plays a significant role in building trust and rapport with patients. A warm, approachable demeanour ensuring a private, welcoming space for discussions can make all the difference in a patient’s comfort level. For IRs, being mindful of their non-verbal cues and ensuring their body language is open and inviting can reinforce their verbal communication, making patients feel more at ease and supported.
Internet-based health information: dealing with patients’ knowledge and expectations
In today’s digital age, patients often arrive at consultations armed with information sourced from the internet. This can set unrealistic expectations or spread misinformation. IRs need to navigate these conversations with empathy, correcting inaccuracies without dismissing the patient’s efforts to understand their condition. Encouraging patients to seek information from reputable sources and offering to provide or recommend resources can help manage expectations and improve understanding.
Tips for working with cancer patients and their families
Cancer diagnosis brings a unique set of emotional and psychological challenges for patients and their families. Communication in this context requires a delicate balanced optimism with honesty, ensuring patients and families are prepared for all outcomes. By delivering truthful information about diagnoses, treatment options, and prognoses, IRs should encourage an open dialogue making space for patients and their families to express their fears, concerns, and wishes. Recognizing the family’s role in the patient’s journey and involving them in conversations can foster a supportive care network (e.g. support groups, psychological counselling) crucial for the patient’s wellbeing.
Tips for working with referring colleagues
Collaboration with referring colleagues is paramount in ensuring cohesive patient care. A clear, concise communication with referring colleagues is essential and characterized by clarity in reports and recommendations, avoiding ambiguity. Sharing information, respecting each other’s expertise, and maintaining a respectful dialogue, as well as establishing information channels and feed-back loops (e.g. MDT-boards, joint electronic health record) can enhance patient outcomes and professional relationships.
As interventional radiology continues to evolve, so too must the communication skills of those who practice it. By focusing on clear, compassionate, and patient-centred communication, IRs can significantly enhance the patient experience, improve treatment outcomes, and foster stronger relationships within the healthcare community.